#3 Longevity 101
The basics of the medical field dedicated to keeping us healthier for longer.
For many, longevity is the first thing that comes to mind when they think about aging. Longevity medicine, or the science of interventions that can help people live longer and healthier lives, is relevant to everyone, regardless of age and health.
I think it’s important to highlight that longevity is meant to address both longer and healthier lives, as we all want to improve not just our lifespan, but more importantly, our healthspan. In Greek mythology, Zeus granted Tithonus the gift of immortality, but not the gift of eternal youth. This led to immense suffering as Tithonus continued to age and decay, unable to die.
In the burgeoning field of longevity, the two issues go hand in hand — longevity science is not only concerned with making you live longer as measured by your chronological age, but more importantly, making you feel younger by your biological age.
Interested in learning more? Professors Alex Zhavoronkov, Evelyne Bischof, and Alexey Moskalev have made it easier to learn about the field of longevity through their online course Longevity Medicine 101. Though the course is targeted for medical professionals, it is also approachable for the general audience.
Here are my key learnings from the course:
Terminology
Fields of Study
Gerontology: An umbrella term for the study of aging processes and older adults from physical, mental, and social perspectives.
Biogerontology: A subfield of gerontology that focuses on biological aging processes, their evolutionary origins, and associated interventions to slow down or reverse biological aging.
Longevity Medicine: Biogerontology applied to clinical practice, typically involving personalized precision therapeutics, where multiple aging clocks are monitored, and systematic interventions are offered for the prevention and treatment of chronic diseases. This is not yet formally recognized as a medical discipline.
Geriatric Medicine: Diagnostics and therapeutics in the elderly, including palliative care.
Geroscience: A scientific field that explores the genetic, molecular, and cellular mechanisms that render aging a major driver of age-related diseases and chronic conditions.
Symptoms of Aging
Homeostasis: The ability of an organism to maintain constant internal conditions (e.g., blood acidity, oxygen saturation) under external disturbances. One symptom of aging is the decline in homeostatic capabilities, leading to an increased risk of age-related diseases and death.
Senescence: The process of growing old, particularly at the cellular level. In biology, senescence refers to cells that have aged and permanently stopped dividing but do not die. Over time, large numbers of senescent cells can accumulate in tissues throughout the body.
Inflammaging: Chronic, aseptic, low-grade inflammation that develops with aging and contributes to the pathogenesis of age-related diseases.
Interventions of Aging
Aging Biomarkers: Measurable parameters that qualitatively and quantitatively reflect the rate of human aging.
Geroprotectors: Substances that can reduce the aging rate and increase the healthy lifespan.
The Key Questions of Longevity (Unresolved)
Should aging be treated as a disease?
At first glance, the statement seems preposterous—why should aging be treated as a disease when it is a natural part of the human condition?
However, since modern medicine is based on the evidence-based treatment of symptoms and diseases, advocates argue that this classification is critical for developing therapeutic interventions and preventative strategies targeting aging and age-related diseases.
In 2021, the World Health Organization proposed this change in its International Classification of Diseases (ICD), a catalog used to standardize disease diagnosis worldwide. The plan was to replace the diagnosis of “senility” with the more expansive term of “old age”, and to define the extension code for “aging related” diseased as those “caused by pathological process“, implying that old age could be a disease in itself.
This revision was retracted when the 11th version of the ICD was formally released without references to “old age.” “Aging-related” diseases were categorized as those “caused by biological processes,” removing implications that aging itself could be classified as a disease.
The primary concern about classifying aging as a disease is that it could further ageism and lead to misuse by physicians. Instead of determining exactly what is wrong with a patient, a physician might simply attribute a problem to “old age.”
Regardless of the classification, scientists and researchers continue their quest to address aging.
What is aging?
To complicate matters, scientists do not agree on a universal definition of aging.
At a high level, aging is commonly described as the gradual accumulation of intracellular and extracellular damage or errors that impair the body's functioning at various organizational levels.
Some researchers argue that this accumulation results from the cell's reparative systems being unable to eliminate certain types of damage.
Proponents of programmed aging suggest that aging is driven by evolutionary mechanisms activated at specific stages of development to make room for the next generation. However, no gene, hormone, or body structure has yet been identified as initiating aging in humans.
Another perspective views aging as a quasi-program—a byproduct of the hyperactivation of compensatory mechanisms in response to accumulated damage and errors.
How do we measure aging?
Currently, there are no universal biomarkers of aging besides chronological age. However, we know that there are significant variations in populations with the same chronological age.
This has led to the field of developing aging biomarkers, or metrics that can be used to measure aging in people. An aging biomarker needs to satisfy the following criteria:
High correlation with chronological age in healthy individuals
Can be used to predict mortality better than chronological age
Indicative of the risk of onset for age-relate diseases
Minimally invasive sample collection procedures
Sensitive to early signs of aging, as opposed to mortality and frailty
Low analytic variability, robust and reproducible results
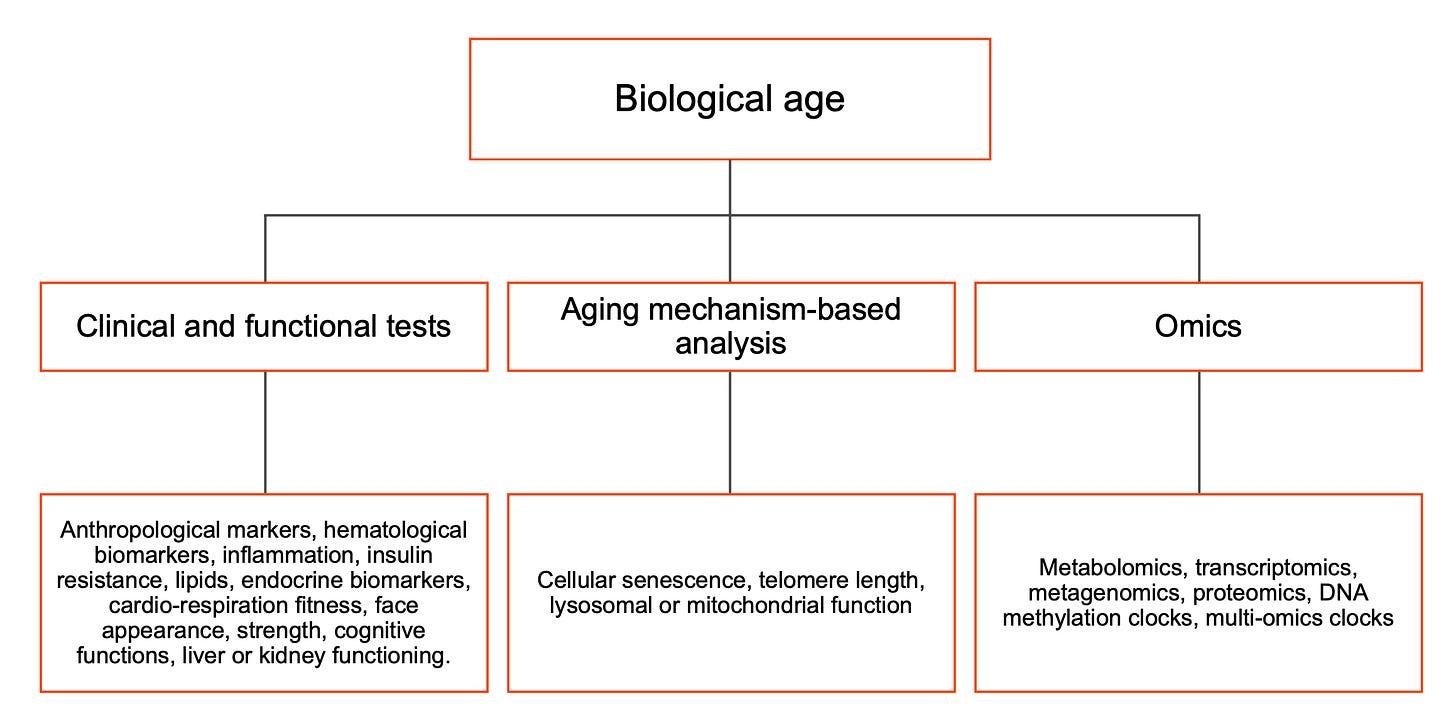
Biomarkers can be measured through three different types of testing:
Clinical and functional: links biological age to specific biological processes
Aging mechanism-based analysis: measures hallmarks of aging through theoretically known mechanisms of aging (e.g., cellular senescence)
Omics: the objective of omics is to identify, characterize, and quantify all biological molecules that are involved in the structure, function, and dynamics of a cell, tissue, or organism. Scientists use data-based approaches train predictors of chronological age with omics data.
Most longevity physicians operate under the assumption that there are multiple aging biomarkers that should be measured and monitored together. This is because each biomarker has its own advantages and limitations.
Areas of Innovation
In addition to the continued search for more aging biomarkers, there is also potential to use neural networks to combine different individual biomarkers together.
How do we study geroprotectors and other interventions of aging?
Aging biomarkers are crucial for establishing standardized methods to measure the effectiveness of anti-aging therapies, or longevity medicine.
Many longevity interventions overlap with general health advice: regular exercise, adequate sleep, and dietary optimization. The most well-known intervention is caloric restriction—reducing calorie intake without compromising overall health.
The more exploratory aspect of longevity medicine is the search for geroprotectors, or substances that aim to reduce the aging rate and prevent the onset of aging-related diseases.
As mentioned before, developing geroprotectors is challenging due to the lack of universally accepted biomarker panels to measure their efficacy. Additionally, most geroprotectors under investigation are gerosuppressors, meaning they may slow aging but cannot reverse it. This makes clinical trials more challenging as it is harder to statistically prove the effectiveness of a substance in slowing a symptom as opposed to reversing it, particularly when the symptom in question is something as complicated as aging.
Areas of Innovation
Scientists have identified hundreds of compounds that could extend lifespan across various organisms. Some geroprotectors have advanced from academic research to clinical trials, including metformin, everolimus, and urolithin.
Unlike geroprotectors, cell therapy offers the potential for true rejuvenation. Induced pluripotent stem cell (iPSC) technology, pioneered by Shinya Yamanaka, has been in clinical trials since 2008 for age-related diseases like macular degeneration, Alzheimer’s, and cancer.
Gene therapy is poised to be the next breakthrough in anti-aging therapeutics. In the future, the concept of a “healthy genome” may emerge, with on-demand allele editing becoming a common approach to achieving it.
Conclusion
Based on this elementary exploration into longevity medicine, it seems to me that the field is still in the early innings of its evolution. The key challenges to this field are not just scientific, but institutional, rooted in how our health care systems develop drugs and therapies. Despite this, investors have shown appetite to pour billions of dollars into this space (link, link). Though I wouldn’t expect longevity medicine to be a reason to negate the need to invest in other areas of AgeTech today, this remains a space worth watching.



